10 Ways to Support Gut Health
Oct 2021

ONE: Start with the basics
Whenever I am asked to consider ways to support individual organ systems or processes (such as brain health, skin health, immunity etc.), I always start by saying that we can’t isolate just one part of the body and focus only on that.
We exist as an intricately connected whole system. What affects one area of our body will also affect everywhere else, to a greater or lesser extent. This concept applies to our gut health. So while there are certain strategies that may specifically benefit our microbiota or digestive health, we must consider their wider effects, too.
Likewise, many aspects of our lifestyle beyond just diet can also influence our gut – from lack of sleep, to stress, to being consistently sedentary. Therefore, perhaps the most important first step to nourishing our gut is actually to nourish our whole body and mind. To establish those fundamental basics of health: restorative sleep, moderate alcohol intake,regular movement, a balanced and nourishing diet, active stress management and social connection.
Often, we may find that when these basics are in place, consistently (not perfectly – that’s not a realistic goal), much of the rest takes care of itself.
TWO: Take time to eat, sit down & chew properly
Our digestion needs time to work properly, so sit down to eat, and try to give yourself at least 10 minutes for each meal, ideally undistracted. The more relaxed we are when eating, the more we activate the ‘rest and digest’ state of our nervous system. Which, as the name suggests, is very helpful to support efficient digestion.
Chew your food well and give your digestion a break between meals (I suggest at least 4-5 hours). These two simple factors can do an awful lot of good when it comes to gut health, especially bloating, without changing a single thing in your diet.
If you’d like more information on how to practice mindful eating (including a mindful exercise) as well as more on digestive health and nutrition, I suggest taking a look at my online course which explores many of these topics in detail.
THREE: Drink enough water
Your body maintains a finely tuned fluid balance by absorbing more water from your gut if you are getting a little dehydrated. This hardens the contents of your bowels, and so dehydration is a common cause of slow gut transit time and constipation.
Good hydration enables good elimination! For gut health, it is suggested that we aim for around 30-25ml fluids per kg of body weight per day (although this will vary according to the temperature and amount of exercise you are doing too, so as always, please listen to your body).
FOUR: Include healthy fats in your diet
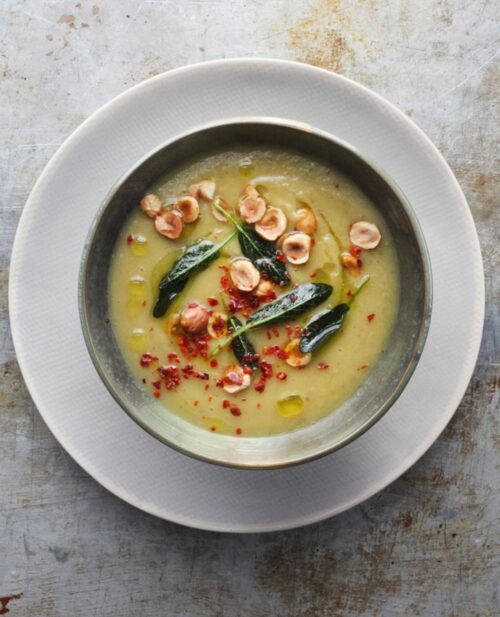
For simplicity’s sake when it comes to healthy fats, I generally recommend using plain olive oil for cooking, and your fancy extra-virgin olive oils for salad dressings and drizzling. Other healthy fats, such as avocados, oily fish and nuts & seeds, are also very gut friendly.
There is a lot more information on how to build a healthy diet, including which healthy fats to go for in my third book, Nourish & Glow: The 10 Day Plan.
FIVE: Focus on fibre
A fibre-rich diet is associated with an increased diversity of the gut microbiota (and, in general, the greater the diversity the better), as well as helping to reduce constipation and other bowel-related problems. It may potentially even help to reduce the risk of heart disease and stroke (Wald, 2013) (Gobson and Shepher, 2010) (De Filippo et al., 2010).
Plus, fibre is filling and low in available calories, so great for those who are watching their weight. Aim for at least 30g/day, which you can get from lots of fresh vegetables, beans and pulses, and unrefined, whole-grain carbohydrates (oats, millet, quinoa, amaranth etc.).
See my article ‘Eat More Fibre’ for lots more on this topic.
SIX: Eat a colourful diet rich in polyphenols
Plant polyphenols are important naturally occurring compounds that are found in a range of plants, fruits and vegetables which are thought to have all sorts of beneficial effects for both your gut and your body as a whole (Puupponen-Pimia et al., 2002).
Good sources of polyphenols include:
Citrus fruits (whole fruits though, not just the juice!).
Dark green leafy vegetables (spinach, chard, cabbage, kale etc)
Red and purple berries (I often recommend a portion a day for gut health – frozen ones are fine when fresh are out of season)
Nuts and seeds. Linseeds (also known as flax seeds) and chia seeds are a good example, although I would recommend soaking them for a few hours or overnight in water before eating them for maximum nutrient absorption. I would suggest trying to have a moderate portion of nuts, seeds or nut butter every day (assuming you tolerate them well and have no allergies)
Cacao – yep, that means chocolate! Either go for raw cacao or organic cocoa powder, or look out for organic chocolate with a cocoa content of > 85%. 10-25g per day is a sensible amount (that’s about 1-2 large squares).
For more information on polyphenols, take a look at my article Why ‘eating the rainbow’ is not just a cliched phrase – also contains lots and lots of colourful recipe inspiration.
SEVEN: Include some probiotic & prebiotic foods
Probiotic foods include organic fermented dairy products such as bio live plain yoghurt, sour cream, aged cheese or kefir (if you tolerate casein protein and lactose). Alternatively, kimchi, kombucha, miso, natto, sauerkraut and tempeh are fermented too. Do make sure that these contain ‘active, live cultures though’ – if they have been pasteurized or heat-treated after fermentation then they will no longer have significant probiotic function.
Prebiotic foods include things like asparagus, under-ripe banana, aubergine, endive, garlic and onions, Jerusalem artichokes, leeks, pulses (such as beans, peas and lentils) and chicory. Unrefined wholegrains may also have some prebiotic function.
Please note: It’s recommended that you always start to include these foods very gradually into your diet. Adding a lot of probiotics and prebiotics at once can potentially lead to a significant exacerbation in gut symptoms. Sometimes I recommend just a teaspoon every other day to begin with (although others may be fine adding more). Listen to your own body, as always.
EIGHT: Consider possible food allergies & intolerances
If you have a specific food allergy or intolerance, this food may need to be eliminated for a while (or indeed, indefinitely in some instances), to allow your gut and symptoms to heal.
It’s always best to speak to a Registered Nutritionist, Nutritional Therapist or Dietitian to advise you on this. As far as possible, eating a widely varied diet is important to ensure we don’t inadvertently develop nutrient insufficiencies, and to minimise the stress and anxiety we might feel around eating.
Please be wary of any online company that offers at-home tests to find if you have any allergies or intolerances – most of these are not proven to be effective, and may result in you restricting your diet unnecessarily.
NINE: Reduce ultra-processed foods
It’s a good idea, both for our overall health as well as for our gut health, to cut down on the amount of heavily processed and/or junk food we consume, especially processed meats and high-sugar, high saturated fat foods. Although all foods do have their rightful place in a balanced diet, moderation is important when it comes to these sorts of foods. It’s best to base the majority of our meals on whole foods, such as fruits, vegetables, high-quality proteins, pulses, wholegrains and nuts & seeds, cooked simply.
TEN: Actively manage stress
Stress can be a big factor in both our gut health and our overall health. Our brain, microbiota and gastrointestinal tract are all intricately connected, and can all affect each other. This book explains that connection really well.
Although we all feel stress, and a bit of it can actually be beneficial to us, too much is definitely unhelpful. Actively managing stress can take many forms. Some people find exercise incredibly helpful, others self care and others still seek social connection in times of challenge.
It’s less about what you do than actually doing it consistently. This book, offers a great deal of ideas, tips and suggestions if you’re not sure where to begin when it comes to reducing your own stress levels.
You’ll find lots of recipes here rich with prebiotic foods – why not give some of these a try?
References & Bibliography:
Please note: This article is for information only and in no way replaces medical or personal nutrition advice. You should always speak to your healthcare provider in the first instance if you have any concerns whatsoever about your digestive or gut health. Please do not disregard or delay treatment based on anything you read on this website. I am not a doctor, nor am I your Nutritional Therapist. The information I share is very general and may not be relevant or appropriate for you as an individual.
Bjarnason, I., Williams, P., Smethurst, P., Peters, T.J. and Levi, A.J. (1986) ‘Effect of non-steroidal anti-inflammatory drugs and prostaglandins on the permeability of the human small intestine’, Gut, 27(11), pp. 1292–1297. doi: 10.1136/gut.27.11.1292.
De Filippo, C., Cavalieri, D., Di Paola, M., Ramazzotti, M., Poullet, J.B. and Massart, S. (2010) ‘Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa’, Proceedings of the National Academy of Sciences, 107(33), pp. 14691–14696. doi: 10.1073/pnas.1005963107.
De-Souza, D.A. and Greene, L.J. (2005) ‘Intestinal permeability and systemic infections in critically ill patients: Effect of glutamine*’, Critical Care Medicine, 33(5), pp. 1125–1135. doi: 10.1097/01.ccm.0000162680.52397.97.
Dethlefsen, L. and Relman, D.A. (2010) ‘Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation’, Proceedings of the National Academy of Sciences, 108(Supplement_1), pp. 4554–4561. doi: 10.1073/pnas.1000087107.
Gibson, P.R. and Shepherd, S.J. (2010) ‘Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach’, Journal of Gastroenterology and Hepatology, 25(2), pp. 252–258.
Lambert, G., Boylan, M., Laventure, J.., Bull, A. and Lanspa, S. (2007) ‘Effect of aspirin and ibuprofen on GI Permeability during exercise’, International Journal of Sports Medicine, 28(9), pp. 722–726. doi: 10.1055/s-2007-964891.
Puupponen-Pimiä, R., Aura, A.., Oksman-Caldentey, K.., Myllärinen, P., Saarela, M., Mattila-Sandholm, T. and Poutanen, K. (2002) ‘Development of functional ingredients for gut health’, Trends in Food Science & Technology, 13(1), pp. 3–11. doi: 10.1016/s0924-2244(02)00020-1.
Wald, A. (2013) Patient information: High-fiber diet (Beyond the Basics. Available at: UpToDate (Accessed: 1 December 2015).
Photos by Jen Rich and Darryl Leja
MORE TO EXPLORE
Please note that the information on this website is provided for general information only, it should not be treated as a substitute for the medical advice of your own doctor or any other health care professional providing personalised nutrition or lifestyle advice. If you have any concerns about your general health, you should contact your local health care provider.
This website uses some carefully selected affiliate links. If you buy through these links, we may earn an affiliate commission, at no additional cost to you. This helps to keep all of our online content free for everyone to access. Thank you.